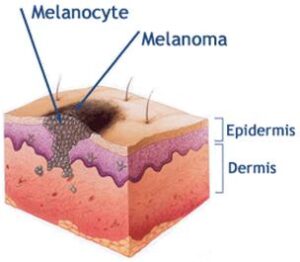
Skin cross-section showing development of a melanoma.
About Melanoma
Melanoma is a cancer of the pigment cells of the skin. Like cancers in other parts of the body, it is composed of cells, which multiply without the normal control of the body’s regulating systems.
Moles and Melanoma
Melanoma can develop within pre-existing moles but also commonly arises within previously normal skin. Change, particularly in the size, border or pigmentation of a mole needs to be carefully evaluated to exclude melanoma. Similarly the developments of new pigmented areas in the skin of adults need to be reviewed for the same reason.

Primary melanoma
After a skin examination remember that all the pigment cells in existing moles and those scattered in the skin retain the potential to become cancerous at some time in the future. Regular self-review is always appropriate and patients should also have expert re-examination periodically.
Risk Factors
- Personal or family history of melanoma
- Multiple moles (>100)
- Dysplastic naevi syndrome
- Fair skin, freckles, blue eyes, red hair
- Severe sunburn or recreational exposure
- Other types of skin cancer
Other forms of skin cancer
The most common types of skin cancer arise from non-pigmented cells (basal and squamous) in the epidermis. These forms of skin cancer need to be managed carefully as they can cause significant problems by invading adjacent tissues. Basal cell carcinomas (BCC) do not spread to the lymph glands or distant sites; squamous cell cancers (SCC) of the skin usually behave similarly.
Management of a suspected melanoma
Once a pigmented lesion has been identified to be of concern the next step is usually to perform a biopsy under local anaesthesia. This is performed in doctors’ rooms and simply consists of removing the lesion with two millimetres of surrounding skin. The pathologist then examines this under the microscope and if melanoma is identified, performs other special tests called micro staging to help determine how abnormal the melanocytes (pigment cells) have become and the extent the tumour may have invaded the layers of the skin. This information will be used to plan subsequent treatment and should allow your doctor to give an indication as to the likely outcome.

Biopsy
Prognosis (the outlook)
The prognosis for patients with melanoma varies from almost certain cure to a much less predictable outlook and is largely dependent on the micro staging of the primary melanoma. Most patients with melanoma thinner than 1mm have an extremely good chance (better than 95%) of being alive and without evidence of further tumour in 10 years. Patients with thicker melanomas have a higher likelihood of developing metastases (secondary deposits of cancer) in the lymph glands or other parts of the body.
Is it possible to determine if the melanoma has spread
Physical examination is useful to detect tumours in most of the lymph node groups.
Other tests such as CT scans or PET scans can also detect metastases (secondaries).
Surgery for primary melanoma
Surgical excision is the mainstay of treatment for melanoma. This surgery is usually straight forward, and frequently the wound results in a simple line scar. On other occasions skin adjacent to the site of the melanoma is used as a flap to close the wound. Much less commonly a skin graft from elsewhere is used to close the wound.
Your Surgeon will discuss with you the indications for lymph node assessment called Sentinel Node Biopsy.
What else needs to be done?
When there is no evidence of spread to other parts of the body, particularly the lymph glands, then it is likely that your doctor will recommend no further treatment. Surgery to remove the lymph nodes which drain the area of a tumour is needed if there is reason to suspect that a tumour has spread there. If other metastases are found, chemotherapy or radiotherapy may be suggested.
The wound
Surgical wounds are often a little red and thick for 6-12 weeks after the operation due to the new blood vessels and collagen in the healing wound. This progressively settles and you will be instructed about the use of creams and ointments to moisturize the young scar and SPF 50+ (“block out “) sun screens to protect the wound from excess sunlight.
Follow up and other tumours
Expert periodic review is very important. Your doctor will decide how regularly this needs to be based on the specific details of your tumour. One of the most common sites where the tumour can reappear is in the lymph node groups (including the arm pit, groin and neck). These will be checked at the review consultations.
If your skin has developed a skin cancer due to the combination of sun exposure and a susceptible skin type, then you may be at risk of developing other tumours. For this reason you should have regular skin surveillance.